The hospitals are eerily quiet, except for Covid-19.
I have heard this sentiment from fellow doctors across the United States and in many other countries. We are all asking: Where are all the patients with heart attacks and stroke? They are missing from our hospitals.
Yale New Haven Hospital, where I work, has almost 300 people stricken with Covid-19, and the numbers keep rising — and yet we are not yet at capacity because of a marked decline in our usual types of patients. In more normal times, we never have so many empty beds.
Our hospital is usually so full that patients wait in gurneys along the walls of the emergency department for a bed to become available on the general wards or even in the intensive care unit. We send people home from the hospital as soon as possible so we can free up beds for those who are waiting. But the pandemic has caused a previously unimaginable shift in the demand for hospital services.
Some of the excess capacity is indeed by design. We canceled elective procedures, though many of those patients never needed hospitalization. We are now providing care at home through telemedicine, but those services are for stable outpatients, not for those who are acutely ill.
What is striking is that many of the emergencies have disappeared. Heart attack and stroke teams, always poised to rush in and save lives, are mostly idle. This is not just at my hospital.
My fellow cardiologists have shared with me that their cardiology consultations have shrunk, except those related to Covid-19. In an informal Twitter poll by @angioplastyorg, an online community of cardiologists, almost half of the respondents reported that they are seeing a 40 percent to 60 percent reduction in admissions for heart attacks; about 20 percent reported more than a 60 percent reduction.
And this is not a phenomenon specific to the United States. Investigators from Spain reported a 40 percent reduction in emergency procedures for heart attacks during the last week of March compared with the period just before the pandemic hit.
And it may not just be heart attacks and strokes. Colleagues on Twitter report a decline in many other emergencies, including acute appendicitis and acute gall bladder disease.
The most concerning possible explanation is that people stay home and suffer rather than risk coming to the hospital and getting infected with coronavirus.
This theory suggests that Covid-19 has instilled fear of face-to-face medical care. As a result, many people with urgent health problems may be opting to remain at home rather than call for help.
And when they do finally seek medical attention, it is often only after their condition has worsened. Doctors from Hong Kong reported an increase in patients coming to the hospital late in the course of their heart attack, when treatment is less likely to be lifesaving.
There are other possible explanations for the missing patients. In this time of social distancing, our meals, social interactions and physical activity patterns tend to be very different.
Maybe we have removed some of the triggers for heart attacks and strokes, like excessive eating and drinking or abrupt periods of physical exertion. This theory merits research but seems unlikely to explain the dramatic changes we’re observing.
We actually expected to see more heart attacks during this time. Respiratory infections typically increase the risk of heart attacks.
Studies suggest that recent respiratory infections can double the risk of a heart attack or stroke.
The risk seems to begin soon after the respiratory infection develops, so any rise in heart attacks or strokes should be evident by now. We urge people to get flu vaccines every year, in part, to protect their hearts.
Also, times of stress increase the risk of heart attacks and strokes.
Depression, anxiety and frustration, feelings that the pandemic might exacerbate, are all associated with a doubling or more of heart attack risks.
Work and life stress, which also may be higher with the acute disruptions we’ve all been going through, can markedly increase the risk of a heart attack.
Moreover, events like earthquakes or terrorist attacks or war, in which an entire society is exposed to a stressor, are risk factors for heart attacks.
Finally, Covid-19 can actually affect the heart, which should be increasing the number of patients with heart problems.
Experts are bringing together data to confirm these patterns. We hope to gain a greater understanding of their causes and consequences.
Meanwhile, the immediate message to patients is clear:
Don’t delay needed treatment.
If fear of the pandemic leads people to delay or avoid care, then the death rate will extend far beyond those directly infected by the virus.
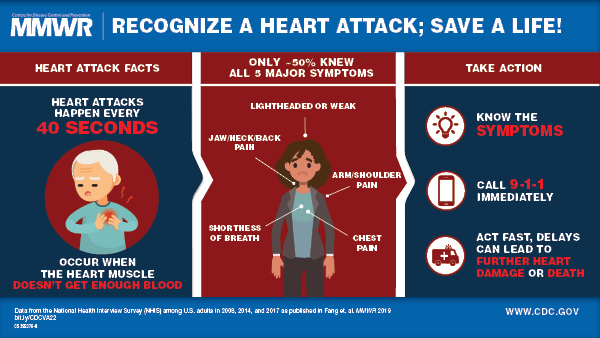
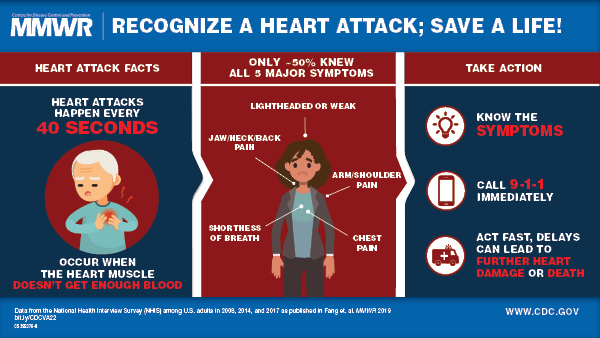
Time to treatment dictates the outcomes for people with heart attacks and strokes. These deaths may not be labeled Covid-19 deaths, but surely, they are collateral damage.
The public needs to know that hospitals are equipped not only to care for people with Covid-19 but also those who have other life-threatening health problems.
Yes, we in health care are working to keep people out of the hospital if we can, but we can safely provide care for those people who are not sick from Covid-19. Masks and protective gear for health care workers and patients go a long way to ensure a safe environment.
Also, people with chronic conditions need to know that avoidance of needed care could ultimately be as big a threat as the virus itself.
As we fight coronavirus, we need to combat perceptions that everyone else must stay away from the hospital. The pandemic toll will be much worse if it leads people to avoid care for life-threatening, yet treatable, conditions like heart attacks and strokes.
Harlan Krumholz, M.D., is a professor of medicine at Yale and director of the Yale New Haven Hospital Center for Outcomes Research and Evaluation.
more recommended stories
 Fentanyl Seizures at Border Continue to Spike, Making San Diego a National Epicenter for Fentanyl Trafficking
Fentanyl Seizures at Border Continue to Spike, Making San Diego a National Epicenter for Fentanyl TraffickingFentanyl Seizures at Border Continue to.
 Utah Man Sentenced for Hate Crime Attack of Three Men
Utah Man Sentenced for Hate Crime Attack of Three MenTuesday, August 8, 2023 A.
 Green Energy Company Biden Hosted At White House Files For Bankruptcy
Green Energy Company Biden Hosted At White House Files For BankruptcyAug 7 (Reuters) – Electric-vehicle parts.
 Former ABC News Reporter Who “Debunked” Pizzagate Pleads Guilty of Possessing Child pδrn
Former ABC News Reporter Who “Debunked” Pizzagate Pleads Guilty of Possessing Child pδrnFriday, July 21, 2023 A former.
 Six Harvard Medical School and an Arkansas mortuary Charged With Trafficking In Stolen Human Remains
Six Harvard Medical School and an Arkansas mortuary Charged With Trafficking In Stolen Human RemainsSCRANTON – The United States.
 Over 300 People Facing Federal Charges For Crimes Committed During Nationwide Demonstrations
Over 300 People Facing Federal Charges For Crimes Committed During Nationwide DemonstrationsThe Department of Justice announced that.
